Too few governments levy appropriate levels of tax on
cigarettes and other tobacco products. They therefore miss out on a
proven, low-cost measure to curb demand for tobacco, save lives and
generate funds for stronger health services, according to the "WHO Report on the global tobacco epidemic 2015".
The report focuses on raising taxes on tobacco. Although 33
countries impose taxes that represent more than 75% of the retail price
of a packet of cigarettes, many countries have extremely low tax rates.
Some have no special tax on tobacco products at all.
“Raising taxes on tobacco products is one of the most
effective – and cost-effective – ways to reduce consumption of products
that kill, while also generating substantial revenue,” says Dr Margaret
Chan, WHO Director-General. “I encourage all governments to look at the
evidence, not the industry’s arguments, and adopt one of the best
win-win policy options available for health.”
Strategies to support the implementation of demand reduction
measures contained within the WHO Framework Convention on Tobacco
Control (WHO FCTC), such as the “MPOWER” package, have helped save
millions of lives in the past decade. MPOWER was established in 2008 to
promote government action on 6 tobacco control strategies – 1 for each
letter of the MPOWER acronym – to stamp out the tobacco epidemic, namely
to:
- Monitor tobacco use and prevention policies;
- Protect people from tobacco smoke;
- Offer help to quit tobacco use;
- Warn people about the dangers of tobacco;
- Enforce bans on tobacco advertising, promotion and sponsorship; and
- Raise taxes on tobacco.
The main findings of the report, funded by Bloomberg
Philanthropies, include the fact that raising taxes is the least
implemented MPOWER measure in terms of population coverage, and the one
that has seen the least improvement in terms of government action since
2008. However, by 2014, 11 countries had raised taxes so that they
represent more than 75% of the retail price of a packet of cigarettes,
joining the 22 countries that had similarly high taxes in place in 2008.
Dr Douglas Bettcher, Director of WHO’s Department for the
Prevention of Noncommunicable Diseases (NCDs), says higher tobacco taxes
and prices are proven methods to reduce consumption and promote
quitting the use of tobacco products.
“Evidence from countries such as China and France shows that
higher tobacco product prices linked to increased taxes lead to declines
in smoking prevalence and tobacco-related harm, such as lung cancer
deaths,” says Dr Bettcher.
Dr Vera da Costa e Silva, Head of the WHO FCTC Secretariat,
notes that the Convention offers governments policies to curb illicit
trade in tobacco products to reduce demand and boost tax revenues from
tobacco sales. “Countries should consider implementing the provisions of
the Protocol to Eliminate Illicit Trade in Tobacco Products to confront
the illegal market,” she adds.
Tobacco taxation could also be a key source of funding for implementing the post-2015 Sustainable Development Goals.
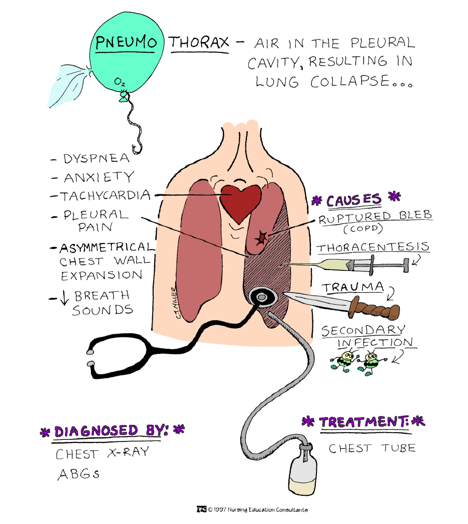
Tobacco-related illness is one of the biggest public health
threats the world has ever faced. Approximately 1 person dies from a
tobacco-related disease every 6 seconds, equivalent to around 6 million
people a year. That is forecast to rise to more than 8 million people a
year by 2030, unless strong measures are taken to control the epidemic.
Tobacco use is also one of the 4 main risk factors behind the
global epidemic of noncommunicable diseases, primarily cancers,
cardiovascular and lung diseases, and diabetes. In 2012, these diseases
killed 16 million people prematurely (before the age of 70 years), with
more than 80% occurring in low- and middle-income countries.